There should be no confusion when dealing with Ebola at hospitals or other locations:
The CDC, NIH under the Department of Health and Human Services wrote the BMBL (Biosafety in Microbiological and Biomedical Laboratories). This is touted as the corner stone of good biosafety practices and is used and followed in Biotechs and research facilities.
I am an EH&S manager (also a radiation safety officer) for a biotech (handling BSL1, BSL2 and rDNA, lentivirus and Adenoviruses using more skin protection BSL2+) and we follow these practices to safeguard the employees and to ensure that we handle, transport and dispose of infectious materials safely.
Under the BMBL 5th edition, Ebola is considered a BSL-4 requiring BSL-4 containment (BioSafety Level - 4) ? ? work with dangerous and exotic agents that pose a high individual risk of aerosol-transmitted laboratory infections and life-threatening disease that is frequently fatal, for which there are no vaccines or treatments, or a related agent with unknown risk of transmission. Agents with a close or identical antigenic relationship to agents requiring BSL-4 containment must be handled at this level until sufficient data are obtained either to confirm continued work at this level, or re-designate the level. Laboratory staff must have specific and thorough training in handling extremely hazardous infectious agents. Laboratory staff must understand the primary and secondary containment functions of standard and special practices, containment equipment, and laboratory design characteristics. All laboratory staff and supervisors must be competent in handling agents and Procedures.? http://www.cdc.gov/biosafety/publications/bmbl5/
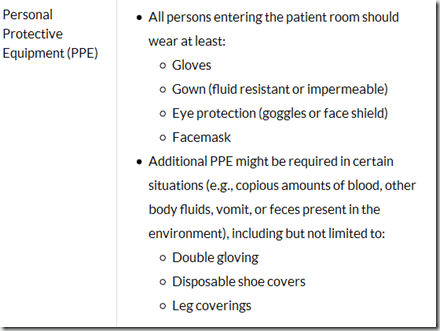
The safety guidelines identify Personal Protective Equipment (PPE), primary and secondary barriers and the design of the laboratory and exhaust. As a biotech we follow these practices.
As a Practicing EH&S manager we train the employees that aerosols can occur during pipetting and any transference of liquids or for any large spill or damaged centrifuge rotors and tubes, whether biological, chemical or radiation. We caution employees to use engineering controls such as Fume Hoods and Biosafety cabinets when working with these substances and that if a spill occurs or a centrifuge has a problem we want them to protect themselves from the aerosol and we want them to leave the area immediately (or wait 20 minutes before opening the centrifuge), after a waiting period we allow re-entry, usually by the EHS response team.
These protection practices are used successfully in every day operations by many industries.
Photo opportunities or incorrect training:
Another thing, I have seen many photos of customs or other agents wearing PPE and looking directly at the person they are interviewing. The PPE is incorrectly used! The pictures I have seen indicate employees wearing surgical masks and in their normal clothes or uniforms with exposed skin.
Caution: I am not complaining that these employees should be wearing hazmat suits and I understand that the photo opportunities may be rushed and they wear whatever is available. The message to the public is wrong and serves to fuel conspiracy theories and a strain on the trust of the employer/employee relationship.
First, hopefully there was a risk assessment completed and documented? The problem with these photos is surgical masks DO NOT protect you against others. An N95 respiratory mask would be more beneficial. Second, designate teams for the interviewing (reducing the numbers of potential exposed personnel). This also reduces the number for medical surveillance. A disposable apron/smock with sleeve covers (scrubs with a laundering service) in case someone was to sneeze would protect the working clothes also a procedure to launder if an incident were to happen should be implemented. Safety glasses are good practices and having the person you are interviewing face to the side would be helpful.
The CDC, NIH under the Department of Health and Human Services wrote the BMBL (Biosafety in Microbiological and Biomedical Laboratories). This is touted as the corner stone of good biosafety practices and is used and followed in Biotechs and research facilities.
I am an EH&S manager (also a radiation safety officer) for a biotech (handling BSL1, BSL2 and rDNA, lentivirus and Adenoviruses using more skin protection BSL2+) and we follow these practices to safeguard the employees and to ensure that we handle, transport and dispose of infectious materials safely.
Under the BMBL 5th edition, Ebola is considered a BSL-4 requiring BSL-4 containment (BioSafety Level - 4) ? ? work with dangerous and exotic agents that pose a high individual risk of aerosol-transmitted laboratory infections and life-threatening disease that is frequently fatal, for which there are no vaccines or treatments, or a related agent with unknown risk of transmission. Agents with a close or identical antigenic relationship to agents requiring BSL-4 containment must be handled at this level until sufficient data are obtained either to confirm continued work at this level, or re-designate the level. Laboratory staff must have specific and thorough training in handling extremely hazardous infectious agents. Laboratory staff must understand the primary and secondary containment functions of standard and special practices, containment equipment, and laboratory design characteristics. All laboratory staff and supervisors must be competent in handling agents and Procedures.? http://www.cdc.gov/biosafety/publications/bmbl5/
The safety guidelines identify Personal Protective Equipment (PPE), primary and secondary barriers and the design of the laboratory and exhaust. As a biotech we follow these practices.
As a Practicing EH&S manager we train the employees that aerosols can occur during pipetting and any transference of liquids or for any large spill or damaged centrifuge rotors and tubes, whether biological, chemical or radiation. We caution employees to use engineering controls such as Fume Hoods and Biosafety cabinets when working with these substances and that if a spill occurs or a centrifuge has a problem we want them to protect themselves from the aerosol and we want them to leave the area immediately (or wait 20 minutes before opening the centrifuge), after a waiting period we allow re-entry, usually by the EHS response team.
These protection practices are used successfully in every day operations by many industries.
Photo opportunities or incorrect training:
Another thing, I have seen many photos of customs or other agents wearing PPE and looking directly at the person they are interviewing. The PPE is incorrectly used! The pictures I have seen indicate employees wearing surgical masks and in their normal clothes or uniforms with exposed skin.
Caution: I am not complaining that these employees should be wearing hazmat suits and I understand that the photo opportunities may be rushed and they wear whatever is available. The message to the public is wrong and serves to fuel conspiracy theories and a strain on the trust of the employer/employee relationship.
First, hopefully there was a risk assessment completed and documented? The problem with these photos is surgical masks DO NOT protect you against others. An N95 respiratory mask would be more beneficial. Second, designate teams for the interviewing (reducing the numbers of potential exposed personnel). This also reduces the number for medical surveillance. A disposable apron/smock with sleeve covers (scrubs with a laundering service) in case someone was to sneeze would protect the working clothes also a procedure to launder if an incident were to happen should be implemented. Safety glasses are good practices and having the person you are interviewing face to the side would be helpful.

Comment